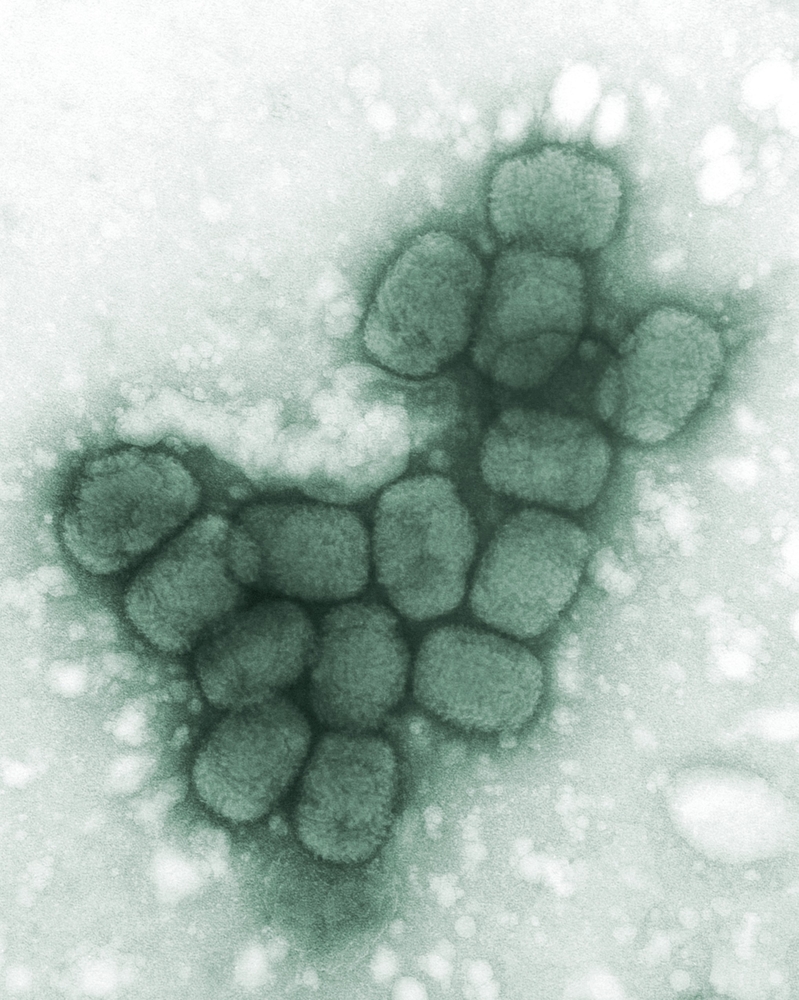
Experts determined during a recently completed hypothetical bioterrorism scenario, which imagines a smallpox outbreak originating in Fiji, that ample preparedness and response capabilities dictate whether a local outbreak is containable or more likely to become a global pandemic.
“Smallpox is spread through the air and is more than twice as infectious as influenza or Ebola. In the case of a biowarfare event, our modeling shows that without a rapid and coordinated response, the epidemic would quickly spiral out of control and become a pandemic,” said Raina MacIntyre, professor of infectious diseases epidemiology at Australia’s University of New South Wales (UNSW) Sydney, who designed the hypothetical smallpox exercise.
Professor MacIntyre, an international expert known for her research on the transmission and prevention of infectious diseases, particularly bioterrorism agents, respiratory pathogens and vaccine-preventable infections, told Homeland Preparedness News last week that pandemics by their very nature can’t be controlled or managed within geographic borders.
“So it is critical that all efforts and resources are focused on the source of the epidemic, and on areas of the world which are struggling to achieve control because an uncontrolled epidemic in one country will inevitably affect all other countries,” she wrote in an email.
“Even in the U.S., which has enough vaccine for its population, a pandemic of smallpox would affect critical supply chains to the country, to all industries and sectors, and travel and trade impacts would be substantial,” said MacIntyre, the principal research fellow at the National Health and Medical Research Council (NHMRC), which is Australia’s expert body on public health standards.
MacIntyre also is director of the NHMRC Centre for Research Excellence in Integrated Systems for Epidemic Response (ISER) at UNSW Medicine’s School of Public Health and Community Medicine. ISER funded the August 16-17 simulated outbreak along with Gaithersburg, Maryland–based global life sciences company Emergent BioSolutions and the Denmark biotech company, Bavarian Nordic.
“There is very little immunity to smallpox in today’s population, so anyone who came into contact with smallpox would need to be vaccinated within three to four days of contact to reduce the risk of serious infection and death,” explained MacIntyre, who heads the biosecurity program at the Kirby Institute.
“Our coordinated regional response should start within seven days of identifying the first case to ensure the best possible outcome and early termination of the epidemic,” she said.
But is that an impossible deadline to meet?
“There is not enough vaccine in the world — estimated to be about 700 million doses presently — to control a worst-case scenario pandemic,” MacIntyre told Homeland Preparedness News. “Manufacturing of vaccines will take another 12-18 months, which is a catastrophic delay.”
But she noted that “if there is a vaccine shortage, the vaccine can be diluted and used in lower doses. If the estimated 700 million doses in the world were distributed equitably and to areas of need rather than held domestically in countries which have stockpiles, there would be enough vaccines for the world.”
The World Health Organization (WHO) now has a stockpile of 35 million doses of smallpox vaccine, but the bulk of it comprises pledged doses from nation states, said MacIntyre.
In a pandemic, when all countries have domestic cases of smallpox, she said the smallpox simulation held at UNSW Sydney was designed to ask: Would countries release their pledged doses to another country in need?
Participants in the scenario included international representatives from health departments, foreign affairs, defense, law enforcement, non-government agencies, and vaccine manufacturers, among other stakeholders who were tasked with finding the answer to that question.
“We felt this was a potential weakness,” MacIntyre explained. “In addition, a pandemic of this scale would affect workforces and economies globally, with supply chains disrupted and high rates of absenteeism in all industries.”
Scenario participants uncovered that for a disease as infectious as smallpox, timing is crucial.
“We have seen in [this] exercise that safeguarding the population against public health threats, whether by accidental, intentional or naturally occurring causes, requires coordinated strategies at the national level,” said Dr. Kevin Yeo, director of clinical and medical affairs at Emergent BioSolutions, in a statement.
“Collaboration across stakeholders and input from experts from government, defense agencies, academia, industry, first responder groups, health care providers, community partners, vaccine manufacturers, and others are key to prepare for, prevent and protect against these threats,” Yeo said, adding that it’s “vitally important for all countries to have a preparedness plan for such untoward events.”
Yet, it’s a mammoth task to ensure health systems closely partner with all of these groups, said David Heslop, associate professor at UNSW Medicine’s School of Public Health and Community Medicine, who helped MacIntyre design the smallpox simulation.
“Whilst the probability of a smallpox attack may be low, the impact will be high, and so it is essential we prepare for these scenarios and know exactly what we can do to avoid the worst occurring,” said Heslop, who is also a senior medical advisor for the Australian Defence Force. “We looked at a worst-case scenario because the purpose of an exercise like this is to prepare for the worst while hoping for the best.”
Overall, scenario participants found that the most important determinants impacting a spread of the epidemic included finding and isolating people with smallpox, tracking their contacts so they could also be vaccinated, and the speed of response.
Detailed simulation outcomes
In an email to Homeland Preparedness News, MacIntyre explained that the simulated smallpox attack in Fiji, a Pacific Island nation with less than a million people, was followed by a hypothetical attack in a larger Asian country. The disease then spread worldwide.
In testing the global responses to the pretend smallpox pandemic, she said many preventable delays surfaced, including those for diagnosis and vaccination “because the vaccinators themselves need to be vaccinated before they commence vaccination.”
Hospital beds also ran out early in the simulated scenario. “Without immediate plans for large-scale isolation facilities (such as using school halls, sports stadiums or hotels), the epidemic can blow out,” she wrote.
Human resources also quickly depleted as health workers themselves succumbed to smallpox. “We would also need rapid plans to mobilize community volunteers to help find cases of smallpox and trace their contacts,” MacIntyre said.
“During eradication, community volunteers were trained for these roles, and also to vaccinate. We need rapid plans to communicate with, engage and work with affected communities in such an event,” she told HPN.
Professor MacIntyre’s hypothetical scenario coincided with new research from UNSW and the PLuS Alliance that shows how minimal genetic material could be used to quickly identify severity and find global transmission routes. Based on previous UNSW research that was adapted to Fiji and the Pacific Island region, the simulation also included lessons learned from real outbreaks.
“Even though the world successfully eradicated smallpox in 1980, the disease has been on the radar again since scientists used mail order DNA to create a virus very similar to smallpox in a lab in 2017,” MacIntyre said, pointing out that the modeled death rate for smallpox could be as high as 45 percent if it emerged today.
In the event of a global pandemic, first responders would need to isolate 70 percent of smallpox patients and track and vaccinate at least 70 percent of their contacts. If the rate dropped to less than 53 percent, bringing the epidemic under control would take over four years and two billion doses of vaccine.
And while the existing WHO stockpile of 35 million doses of vaccine could be diluted in such an emergency, resources to effect large-scale isolation and quarantine would remain the biggest challenges, MacIntyre said.
Counting up challenges
Another challenge would be the myriad situations that could result from such a pandemic, said participant Michael Baker, a professor at the University of Otago in Wellington, New Zealand.
“This has been a vivid reminder that bioterrorism threats are on the radar and has illustrated how a virus such as smallpox might behave in in a world where the population is immunologically vulnerable,” Baker said. “While we cannot prepare totally for all of them, by working through individual case studies, we can produce the concepts and understand the science of working with multidisciplinary teams to prepare for these kind of threats.”
Yet another challenge regarded the issue of surge capacity, according to participant Bill Rawlinson, director of the serology and virology division of the donor screening laboratory at South Eastern Area Laboratory Services, an NSW government initiative.
“Diagnosis can often get left behind, so it is vital that we understand that smallpox is one of many issues in which we must maintain capacity and knowledge around research and development because this is an area that is changing very quickly,” Rawlinson said.
“The other thing that has arisen here is that infrastructure must be tailored to address threats present in diverse circumstances, particularly the threat of a major health crisis in a resource-limited country,” he added.
Professor MacIntyre said certain terrorist groups have called for real biological attacks that could mirror her simulation. And along with their intent, she said there’s also capability for such an attack, although it’s difficult to ascertain who does or doesn’t have such capabilities.
“But we must prepare for the possibility,” MacIntyre said. “Advances in genetic engineering and synthetic biology have increased the risk of such an attack.”
Coordination among countries is essential “from every perspective, whether it be intelligence gathering to prevent a planned attack, to responding to an actual attack, or controlling an established pandemic,” she said.
The difference between terrorism and bioterrorism, the professor explained, is that in the latter, the weapon is invisible, and infection of one or a few people with a highly infectious pathogen could transmit to others, creating an epidemic without any further action required by the perpetrator.
“This can then spread around the world in weeks. We modeled a worst-case scenario, and in this case, the impact on the world would be worse than a nuclear attack and it would take over four years to control the epidemic,” MacIntyre said.




